(In all cases below, the visits were done remotely via phone and Wechat)
Case 1.
Patient: Maggie X, female, 36 years old.
Date: First visit was on March 22, 2020.
Chief complaints: Dry cough and dry, sore throat for one week. Obvious chest distention and pain, with a small amount of nasal mucus in the past two days.
Present ill history: A few days before the onset of illness, Maggie had direct contact with a person in office who was confirmed with COVID-19. Her employer asked her to quarantine at home.
She complained she had dry cough and sore throat for one week. For the past two days, she had obvious chest distention and pain, in addition to dry cough, sore painful throat, sore eyes and mouth with a burning sensation, and a small amount of nasal mucus. Appetite was reduced slightly. No fever. Urine and bowl movements were fine.
Past ill history: Generally healthy. Digestion is not strong enough.
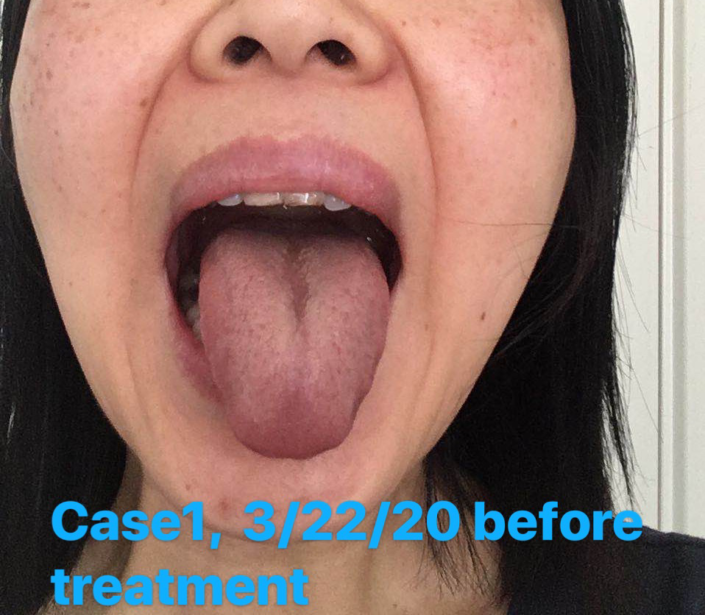
Check the tongue picture: The picture shows red tongue with thin yellow greasy coating and peeling in the middle, and sublingual veins were slightly purple.
Differentiation diagnosis: Yin deficiency with internal heat, evil heat with dampness, blood stasis, and lung Qi does not spread.
Treatments: Recipe–Modified combination of Sang Ju Yin and Ma Xing Shi Gan Tang to clear and ventilate the lung, plus herbs to supplement lung Yin and activate blood:
Sheng Ma Huang 6 Bai He 9 Shan Yao 9 Shi Gao 30 Huang Qin 6
Jin Ying Hua 9 She Gan 6 Sang Ye 9 Chi Shao 12 Shan Zha 6 Zhi Gan Cao 3
Above herbs all put in 1 bag.
Total: 4 bags(4 dosages), 1 bag/day.
10 herb cigarettes: 1-2 herb cigarettes per day to help clear the lungs.
Date: Follow-up on March 24, 2020.
Response to the last treatment: There are major improvements after 2 nd dosage:
1). Dryness and soreness of throat disappeared. The throat has mild itchy feeling.
2). Dry cough, and chest distention and pain have both reduced more than 50%.
3). No nasal mucus.
Check the tongue picture: The tongue changed from purple red to light, with very thin greasy coating.
Treatments: Add Yi Yi Ren 30g to each dosage of the remaining herb or to daily food.
Date: Follow-up on March 25, 2020.
Response to the last treatment: Similar to yesterday. There were some discomfort in
throat, and felt some hot sensation in mouth. After smoking of the medical cigarettes, she felt
relief of chest distention and pain.
Treatments: Continue the same treatment as yesterday.
Date: Follow-up on March 27, 2020.
Response to the last treatment: After 4 dosage of the herb formula and herb
cigarettes, the main symptoms disappeared. The patient considered herself recovered, and
wanted to pause the treatment.
Check the tongue picture: The tongue showed less dampness and heat, with mild blood
stasis.
Treatments: Pause the treatment as the patient wanted. Should follow up later.
Date: Follow-up on April 14, 2020.
Response : The patient reported that everything was fine.
Case 2.
Patient: Jiang X, Female, 42 years old
Date: First visit was on 3/23/2020
Chief complaints: Cough for 10 days, sometimes with white sticky sputum. There are chest pain and loss of smell in recent days.
Present ill history: A few days before the onset of the illness, she had contacted multiple COVID-19 patients at work. Since then she had chest pain, coughing, and loss of smell. The sputum were difficult to cough out, and once out, they were white and sticky. Her western medical doctor prescribed chloroquine and azithromycin. However, these medicine caused stomachache and severe diarrhea to almost exhaustion so that she almost called 911. Therefore, she wanted to consult a Chinese medicine doctor. Now she still have chest pain, coughing with hard-to-cough sputum, and loss of smell. Body temperature and appetite were both fine. No diarrhea after stopping chloroquine and azithromycin.
Past ill history: Generally healthy.
Check the tongue picture: The body of the tongue was pale and slightly bigger, with thick, greasy coating.
Differentiation diagnosis: Damp and cold encumber the lung, and the lung Qi does not spread.
Treatments: Disperse the lung Qi, warm the lung and dissolve phlegm..
Initially I wanted to prescribe her a modified Xiao Qing Long Tang. However, she had told me multiple times that she had already had food therapy such as large amount of ginger and garlic, and she had Chinese herb at home, she didn’t want to drink more herb teas. So my prescriptions to her were:
1) Smell the herb packs that I made to expel the dampness and to avoid the plague using aromatic herbs.
2) Smoke the herb cigarettes that I made to clean dampness and promote blood circulation to cleaning the lungs
Date: Follow-up at the night of March 24, 2020.
Response to the last treatment: After two days of smoking the herb cigarettes:
1). Cough was relieved and the sputum was easy to come out;
2). Chest pain was reduced or even disappeared.
Date: Follow-up on March 25, 2020.
Response to the last treatment: Continued the herb pack and herb cigarettes, results were similar to yesterday. Smell was sometimes good and sometimes bad.
Date: Follow-up on March 27, 2020.
Response to the last treatment: She said that she had received a lot of Chinese herb medicine from China and plan to take them. Stopped the current treatment
Case 3.
Patient: Boy, Amily’s son, 8 years old
Date: First visit was on 3/26/2020
Chief complaints: Dry cough, and change in sense of smell for two days.
Present ill history: Several days before the onset of the illness, he with his mother went to supermarket, but had not contacted with any known COVID-19 patients. His sense of smell and taste changed in recent two days. He always felt that there was a smell in the room, and the milk smelled too. Then he started dry cough. Body temperature was 37.5 c. Last night, he had vomited eight times. He did not feel well in his stomach this morning. Still feel nausea and no appetite. No history of unclean eating.
Past ill history: Generally healthy. Half year ago he had cough for long time.
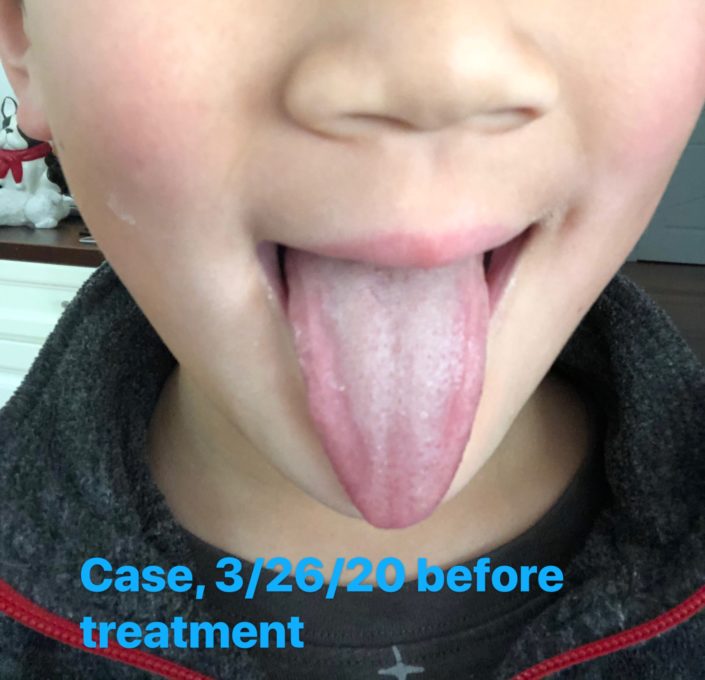
Check the tongue picture:
Tongue was pink with a little thick greasy white coating.
Differentiation diagnosis: Cold and dampness encumber the lung and the stomach.
Treatments: Recipe—Modified combination of Ma Huang Tang and Huo Xiang Zheng Qi wan
Sheng Ma Huang 5 Gui Zhi 5 Huo Xiang 9 Chen Pi 6 Ban Xia 6
Fu Lin 6 Lai Fu Zi 9 Sheng Jiang 2 slices Hong Zao 3 pieces Zhi Gan Cao 3
Above herbs all put in 1 bag.
Total: 3 bags, 1 bag/day.
Date: Follow-up on March 27, 2020.
Response to the last treatment: No more vomiting or dry cough after taking one bag of the herb. His appetite was better, and body temperature returned to normal. His sense of smell also seemed to be back to normal, but sense of taste had not completely recovered.
Treatment: Continue taking the prescribed herb.
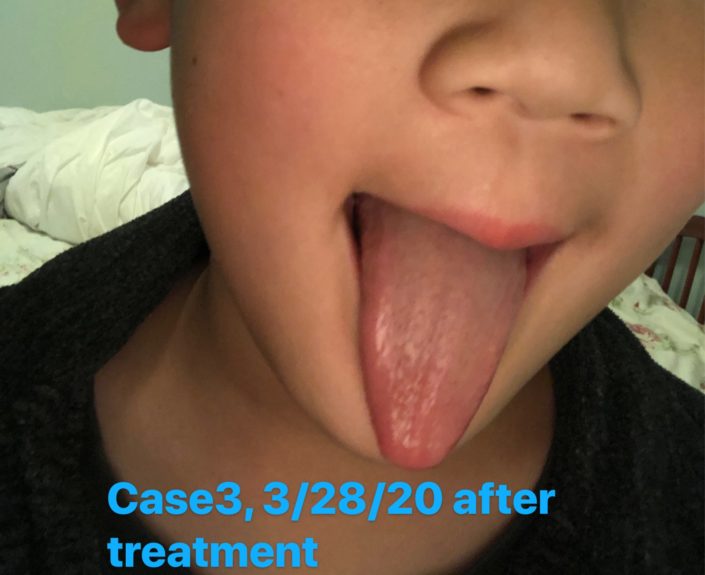
Date: Follow-up on March 28, 2020.
Response to the last treatment: The sense of taste was back to normal. Appetite was normal. Sense of smell was normal. Body temperature was normal. No vomiting or dry cough. His mother said repetitively: “He has recovered. Really recovered.”
Case 4.
Patient: Amily X, Female, 39 years old.
Date: First visit was on 3/26/2020
Chief complaints: Dry cough, sore throat, fear of cold, and alternative chills and fever for one day.
Present ill history: Several days before the onset of the illness, she went to a supermarket. No contact with any known COVID-19 patients. Since last day, she had dry cough, sore throat, fear of cold, and alternative chills and fever. Body temperature was normal. She also had headache, tightness and pain in the back, and loose stools.
Past ill history: Had a history of thyroid cancer surgery.
Check the tongue picture: Tongue was a little red, with tooth marks and slightly yellow greasy coating.
Differentiation diagnosis: Qi and Yin deficiency; dampness-cold was turning dampness-heat, which encumbered the lung and spleen; Ying and Wei were disharmonized.
Treatments: Recipe—Modified combination of Gui Zhi Tang and She Gan Ma Huang Tang, plus herbs to clear the lung, tonify the Qi, and promote the blood circulation.
Sheng Ma Huang 6 Gui Zhi 6 Bai Shao 6 Su Geng 9 She Gan 6
Huang Qin 9 Jin Ying Hua 6 Lai Fu Zi 9 Fresh Ginger 3 slices
Hong Zao 3 pieces Zhi Gan Cao 3
Above herbs all put in 1 bag.
Total: 3 bags, 1 bag/day.
5 herb cigarettes, 1 cigarette /day
Date: Follow-up on March 27, 2020.
Response to the last treatment: After one bag of the herb, loose stools became firm, dry cough disappeared, and tightness of back started to relieve. Still not feel well in the stomach. Forehead was still painful. Still fear of cold. Body temperature was normal.
Treatments: Continue with the above herbs.
Date: Follow-up on March 28, 2020.
Response to the last treatment: Headache and back pain disappeared. Sore throat and fear of cold had relieved.
Treatments: Continue with the above herbs.
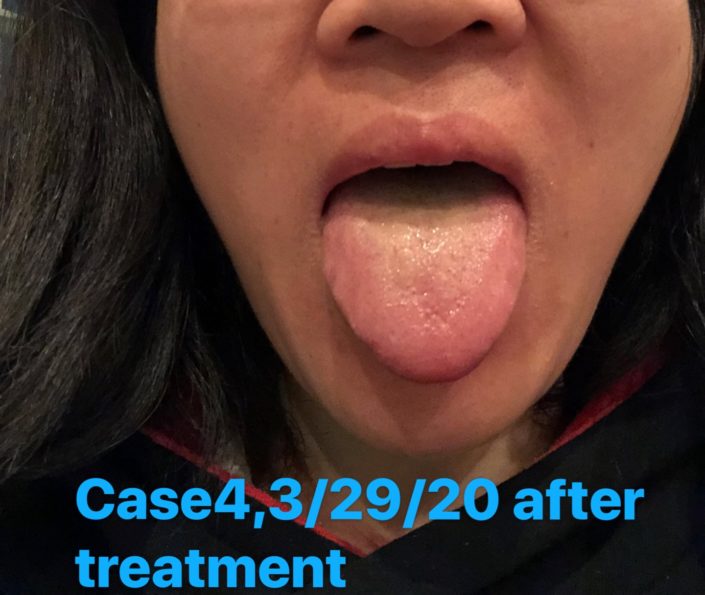
Date: Follow-up on March 29, 2020.
Response to the last treatment: After total of bags of the herb, all symptoms disappeared. Was willing to stop the treatments.
Date: Follow-up on April 15, 2020.
Response to the last treatment: Both herself and her son felt well. Was willing to have an interview by the World Journal.
Case 5.
Patient: Qian X Female, 52 years old
Date: First visit on 4/4/2020
Chief complaints: Fear of cold, headache, and diarrhea for five days. Dizziness, itchy throat, dry cough, and chest distention for two days.
Present ill history: She had contacted someone with COVID-19. Since five days ago, she had fear of cold, headache, and diarrhea. She used some Chinese herbs which reduced headache and diarrhea. However, she had dizziness, itchy throat, chest distention and dry cough starting two days ago. Body temperature normal. Heart beat 101 times/minute.
Past ill history: Mild anemia.
Check the tongue picture: Tongue was pale. The coating was thin white greasy, with yellow in the middle.
Differentiation diagnosis: Dampness-cold encumbered the exterior and invaded the interior. Dampness-cold was turning dampness heat. Lung Qi did not spread.
Treatments: Recipt—A modified combination of Ma Huang Tang and Er Chen Tang, plus some Huang Qin. The principle was resolving dampness and ventilating the lung.
Ma Huang 6 Gui Zhi 6 Ban Xia 6 Chen Pi 6 Fu Lin 9
Huang Qin 6 Su Geng 9 Sheng Jiang 3 pieces Zhi Gan Cao 3
Hong Zao 3 pieces
Above herbs all put in 1 bag.
Total :5 bags 1 bag/day
Date: Follow-up on April 6, 2020.
Response to the last treatment: After taking 3 bags herb tea, fear of cold, itchy throat, dry cough, and dizziness all disappeared. Heartbeat and breathing also became normal. She said, “I only have diarrhea.” Her diarrhea reduced from three times per day to twice per day.
Treatments: Continue the above herb medicine.
Date: Follow-up on April 8, 2020.
Response to the last treatment: After continue taking 2 bags , she felt everything back to normal. She was relaxed and clear-minded. Diarrhea reduced from two to three times per day to once a day, but the stools were still loose. She said that her stool had been loose for a long time, and there was no need to continue treating COVID-19 with the herbs.
Check the tongue picture: The coating was thin and greasy.
Treatments: Suggested that she use fried Yi Yi Ren as food therapy, and come to the clinic to tonify the spleen and stomach after the pandemic.
Date: Follow-up on April 18, 2020.
Response to the last treatment: Everything was normal. She used red beans and Yi Yi Ren porridge. The stools sometimes were formed, and digestion was better than before.
Case 6.
Patient: Jin X , Female, 45 years old.
Date: First visit on 4/10/2020.
Chief complaints: Fear of cold and fever for two days. Diarrhea 13 times starting yesterday.
Present ill history: She was a nurse in hospital and contacted COVID-19 patients. Two days ago she was severely fear of cold, with fever of 100.4 ℉. She took Tylenol every 6 hours to reduce fever. Yesterday when she was calling her friend, she felt dizziness to almost faint. So she called 911 immediately. When the ambulance came, however, the caregivers suggested her to quarantine at home instead. So she took Niu Huang Jie Du Pian pills that was recommended by her friend. Lunch time yesterday she started to diarrhea, and she had that for 13 times by this morning. During diarrhea, there was no abdominal pain, no malodor. She had no history of unclean eating. Now her mouth was dry and loved warm drinks. She felt fatigue, headache, dizziness, and whole body pain. There was no cough, sore throat or breathing difficulty. Her hands were warm but feet were a little cold. She had mild sweat when covered by a heating blanket. Heartbeat was 90/minute. She was conscious. She was afraid of more diarrhea so she seek to Chinese doctors for help.
Past ill history: Easy to feel tired. She had viral meningitis in 2008.
Check the tongue picture: Tongue was pale, red and big. The coating was thin greasy with peeling in middle.
Differentiation diagnosis: Dampness-cold encumbered the exterior and invaded the interior. Dampness-cold was turning dampness heat. Lung Qi did not spread. Qi and Yin deficiency.
Treatments: Ask her to stop Niu Huang Jie Du Pian pills and take electrolyte balanced oral solutions that she bought from market. Rest well. And take the following herbs as soon as possible.
Gui Zhi Ge Gen Tang:
Gui Zhi 6 Bai Shao 6 Ge Gen 12 Fresh Ginger 9 Zhi Gan Cao 6
Hong Zao 6 pieces.
Above herbs all put in 1 bag.
Total: 1 bag today and should follow up tomorrow to modify the recipe as needed.
Date: Follow-up in the morning of April 11, 2020.
Response to the last treatment: Bowl movement twice with stools formed. Diarrhea once. She was much better. However, she still felt chilly, with fever of 100°F in the last evening. So she took Tylenol again to reduce fever.
Check the tongue picture: Tongue was slightly red. The coating was thin, less greasy than before. The peeling in middle disappeared.
Treatments: Add to the previous herb Huo Xiang 9 and Zi Su 9 to further expel external cold and reduce fever, and stop diarrhea by using aromatic herb to resolve dampness. Also ask her to make porridge or tea using fried Yi Yi Ren. Take Vitamin C and electrolyte balanced solutions as supplements. And advised that she should not take Tylenol when the fever was not severe
Total : 3 bags. 1 bag/day
Date: Follow-up on April 12, 2020.
Response to the last treatment: Diarrhea stopped after two days of treatment. No bowl movement today. Last night body temperature was still a little high, but she did not take Tylenol. This morning her body temperature was normal (98.6°F ).
Treatments: continue to take 1 bag of the herbs yesterday prescription
.
Date: Follow-up on April 13, 2020.
Response to the last treatment: One bowl movement today with stools formed. Body temperature normal without fever.
Treatments: She still has one bag of the herbs left. To enhance the treatment effectiveness, asked her to continue take a total of half herb bag a day .
Date: Follow-up on April 14, 2020.
Response to the last treatment: Body temperature normal. Bowl movement once today and it was normal. She complained that her Tai Yang points had some dull pain, which were relieved on pressure. Mouth slightly dry.
Treatments: I did not think the pain on the Tai Yang points were related to wind cold, instead, it should be caused by Qi and Yin deficiency. So I added following herbs to the remaining half dosage:
Dang Shen 9 Mai Dong 9 Wu Wei Zi 6
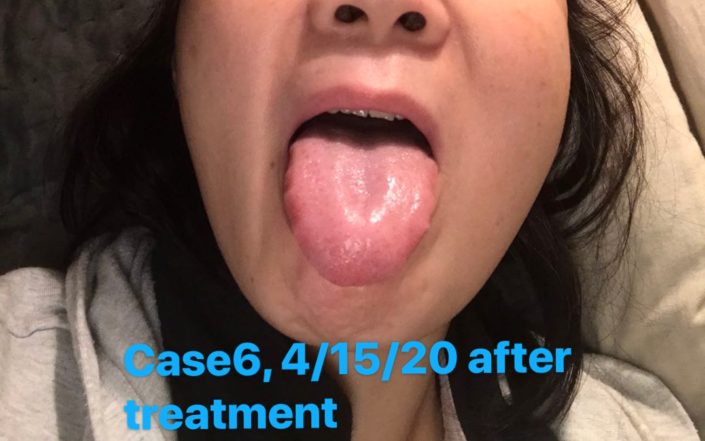
Date: Follow-up on April 15, 2020.
Response to the last treatment: Pain on the Tai Yang points disappeared. Body temperature stayed normal. She said her bowl movements were even better than before when her stools were sticky, but not now. She was very satisfied with the treatments. She said all problems were solved with only 4 dosage of the herbs. She wanted to continue the treatment in order to improve her immune system before going back to work. I suggested that she pause herbs for one day before the next step.
Case 7.
Patient: Jaxon X, Male, 58 years old (He is the husband of the patient in Case 6).
Date: First visit on 4/11/2020.
Chief complaints: In recent three days, he had fear of cold, headache with heavy sensation, a little sneezing, dry cough, tight chest, no appetite, abdominal distension, did not like drink water and vomited after drinking water, and increasing soreness on neck, upper back, and lower back to popliteal fossa .
Present ill history: He had the above symptoms for three days. He also had bitterness in mouth, his breath smelled, his felt head heavy and eyes sight unclear. No sore throat. He felt fever, but body temperature was normal. His stools were sometimes loose. Urine was somewhat yellow. His sleep was more dream and easy to wake up. He was always afraid of the sun and loved cold drinks.
Past ill history: He was diagnosed with depression. He had had panic attack and sense of fear for 7 years. He had superficial gastritis for 2 years, and chronic neck, shoulder, and lower back pain for 4 years.
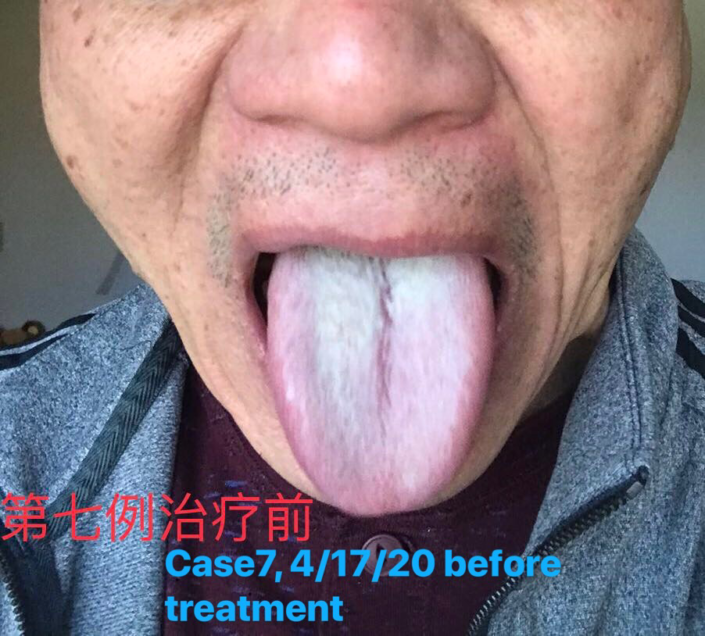
Check the tongue picture: Tongue was dark red with thick white greasy coating.
Differentiation diagnosis: He had Yin deficiency and internal heat, with disharmonized liver and spleen for a long time. Recently he had external cold-dampness and blood stasis.
Treatments: Recipe—Modified Qiu Wei Qiang Huo Tang:
Qiang Huo 9 Du Huo 9 Fang Feng 9 Cang Zhu 9 Huo Xiang 9
Xi Xin 3 Bai Zhi 6 Chuan Xiong 9 Shan Zha 6 Chi Shao 9
Huang Qin 6 Sheng Di 6 Zhi Gan Cao 5 Sheng Jiang 3 pieces.
Above herbs all put in 1 bags
Total 2 bags, 1 bag/day, take 2 times a day.
The case was complicated because he had the new disease and multiple chronicle diseases in the past that were barely improved with medicine for many years. I was concerned that he would have temporary adjustment reactions(“Healing Crisis”) after the herbs, so I warned him and his wife that his symptoms might be slightly worse and there was no need to panic.
Date: Follow-up on April 12, 2020.
Response to the last treatment: As expected, he had some adjustment reactions. No improvements to previous symptoms. Instead, the discomfort was beyond words. Last night he felt irritable, hot and restless during sleep. He had bowl movements twice, with loose stools and strong smell. He was horrified with his status though was warned earlier.
Check the tongue picture: Tongue was red with coating thin greasy (It was a lot better than yesterday )
Treatments: I comfort him again, and asked him to take half dosage of the above herb per day
Date: Follow-up on April 13, 2020.
Response to the last treatment: Irritability was not obvious during sleep last night. Abdominal distension was reduced. He started to want to drink some water, and the feeling vomit after drink disappeared. Still had some dry cough and chest distension (though relieved). Only one of bowl movements had smelly stools, and his abdomen felt much better after the diarrhea.
No relieve of the pain from neck, shoulder to popliteal fossa. He felt the intention to press the popliteal fossa all the time.
Treatments: Finish the remaining half dosage of the herbs.
Date: Follow-up on April 14, 2020.
Response to the last treatment: All symptoms were relieved. No fear of cold, no vomiting when drinking. Appetite normal. Head clear. Still had pain in the Tai Yang points and blurry eyes. Chest distension and shoulder and back pain had reduced. Stools normal.
Combining with tongue pictures, I concluded that the cold-dampness had been mostly resolved.
Treatments: Recipe—Modifyed combine to Qiu Wei Qiang Huo Tang and Xiao Chai Hu Tang. That was, add following to the above prescription.
Chai Hu 12 Dang Shen 9
Total 1 bag. Take 1 bag per day.
Date: Follow-up on April 15, 2020.
Response to the last treatment: Most symptoms were relieved, especially the pain on Tai Yang points and on limbs and shoulder. Still no much improvement on the back pain, so he enjoyed warming up externally using heating water packs. Blurry eyes were better when using fingers to press the eyeballs. A little bitter mouth.
Check the tongue picture: Tongue was a little red. The coating was thin and mild yellow, with grease at the root.
Treatments: Add following herb to the above herbs:
Du Zhong 12 Chuan Duan 12
Total 2 bags, take 1 bag/day.
Date: Follow-up on April 16, 2020
Response to the last treatment: After 2 dosage of the above herb the back pain had reduced. Bitterness in mouth almost disappeared. After 5 dosage of the modified version of above herbs, new symptoms almost all disappeared completely. That concluded this treatment. The patient wanted to move to the next treatment of the chronic disease that had plagued him for a long time.
To Summarize and comment:
1. About “being confirmed”:
All the above patients believed that the got the COVID-19 virus. I encouraged them to do an virus test, but they have not gotten the chance to do so.
1) In California, one needs to have a body temperature of 100℉to be tested.
2) They did not want to expose themselves to a group of highly positive people to infect each other.
3) They were all willing to receive treatments by Chinese medicine to get better sooner and be safer to go back to work.
4) They all felt that their symptoms were different from those of common cold. For example, they had loss of smell or taste without nasal congestion, and chest distention and pain when dry cough beginning or no cough.
5) Five of the above cases have contacted COVID-19 patients. Their tongues were all greasy.
6) Many COVID-19 tests in the United States measured the antibody, which have a good chance of false-positive for patients in early stage of the disease. Some researchers studied the antibody test results in Santa Clara, and estimated that the actual number of COVID-19 patients are 50-85 times more than current confirmed cases.
So, though none of them has the positive test result of COVID-19, they are highly suspected cases and clinically difficult to rule out.
2. About the treatments:
1) Differentiation diagnosis and treatment is the soul of Chinese medicine: Though China has published several agreed prescriptions, such as Qing Fei Bai Du Tang, Xuan Fei Jie Du Tang, Hua Shi Jie Du Tang, Lian Hua Qing Wen Granules, and etc., Chinese medicine requires the doctors to treat the patients based on their individual scenario in order to be efficient and effective.
2) Chinese medicine is not slow. Most of my patients are mild cases, but some were severe like the case with 8 vomiting and 13 diarrhea in less than 24 hours. However, in all cases, patients saw the differences by just one dosage of the herbs, and were all healed by 3-5 dosages.
3. Careful treatments and frequent follow-ups: The plague is raging and venomous. We have to take every suspected cases seriously, especially those with acute symptoms. We should carefully design the best recipe and follow up closely. I sometimes contacted the patients multiple times per day to hear the reactions to the herbs and to understand the progress of the cases. We couldn’t afford to make a mistake.
4. Up to now, most cases were dampness cold. Maybe the cases were still at early to middle stages, or these patients had the habit of eat or drink cold. Some were in the transition from cold to heat, and the treatment strategies should be combined warm up the cold and clear the heat.
(感谢我的学生Vivian Liu 在译文中的协助)